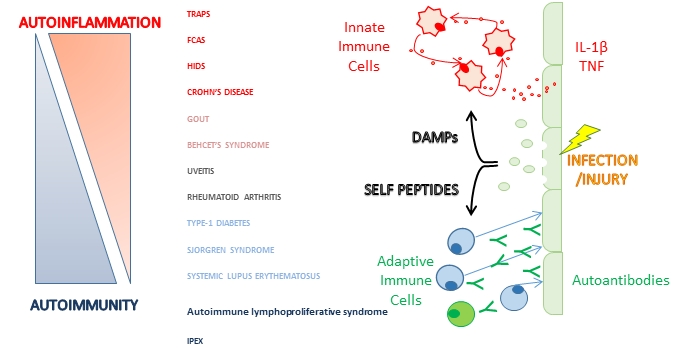
The autoinflammatory disorders, also known as periodic fever syndromes, are a group of diseases that, in their purest forms, manifest as recurrent fevers, high acute phase responses and a proclivity for inflammation of skin, joints, serosal surfaces and other organ involvement including the nervous system. These disorders lack the classical characteristics of autoimmune diseases such as high-titer autoantibodies. The innate immune system plays the primary pathophysiologic role in autoinflammatory diseases and in fact, these diseases are synonymous with dysregulation of the cells and molecular cascades intrinsic to innate immunity.
The periodic fever syndromes are recurring episodes of fever and inflammation (which can be very painful), affecting the abdomen, chest, joints, skin and/or eyes. The inherited diseases (described below) usually present in childhood as does another disease of uncertain cause called PFAPA syndrome. Some of these diseases can also present in adults and Schnizler’s syndrome (also described below) seems to only affect older adults.
Despite similarities in their symptoms, they have differing causes, patterns of inheritance, length and frequency of ‘attacks’. Many of these diseases can now be very effectively treated.
Familial Mediterranean fever (FMF)
Familial Mediterranean fever (FMF) is the commonest of the inherited fever syndromes. It is most often seen in people of Middle Eastern ancestry but can occur in other populations too. It affects both sexes equally and the symptoms usually start in childhood. The disease is thought to affect 1/250 to 1/500 in Sephardic Jews and 1/1,000 in the Turkish population.
The cause of FMF is abnormalities in a gene called MEFV. FMF is a recessive disease meaning that about 85% of patients with FMF have changes (a mutation) in both copies of their MEFV gene. Although 14-25% of patients with a clinical diagnosis of FMF have only one identified mutation, the great majority of individuals with a single mutation are completely healthy carriers. In fact as many as 1 in 4 healthy people in some eastern Mediterranean populations carry an MEFV mutation. This has led to the suggestion that FMF carriers may have had an advantage in the past, possibly that they were less vulnerable to infections.
We are aware of more than 80 different changes (mutations) in MEFV that can cause the disease. Disease causing mutations mostly occur in the part of the gene called exon 10, but we can also find changes in exons 1, 2, 3, 5, 8 and 9.
Attacks of FMF occur irregularly although some people find that minor physical or emotional stress, the menstrual cycle or changes in their diet can cause attacks. Attacks usually last 1 to 3 days with fever and other symptoms. Severe abdominal pain occurs in 85% of cases. Pain which is worse on deep breathing or coughing occurs in 40% of patients, usually only affecting one side of the chest. Severe headache occurs particularly in children, and rarely, in young boys, there can be pain and swelling of the testicles. Muscle and joint pain is common but long term joint damage is very rare. 20% of affected children have muscle pain on exertion, usually affecting the calves even between attacks. A characteristic rash occurs in 20% of patients, usually around the ankles.
Attacks are accompanied by blood test abnormalities showing inflammation, including high white cells, and a very high C-reactive protein (CRP). Investigations may be required to exclude other causes of fever and pain but X-ray, ultrasound or echocardiography during FMF attacks are usually unremarkable.
The diagnosis is supported by gene testing but relies on the history of recurrent short attacks of fever and pain which are accompanied by abnormal blood tests and that are prevented by long term colchicine.
The mainstay of management is long term treatment with low doses of a tablet called colchicine. Continuous treatment with colchicine prevents or substantially reduces symptoms of FMF in at least 95%. How colchicine works remains incompletely understood. Long-term colchicine is advisable in every patient with FMF and vital in those who have AA amyloidosis. Although colchicine is very toxic in acute overdose, the low daily doses required for treatment of FMF are generally very well tolerated by children and adults. Diarrhoea is the most common side effect and can usually be avoided by gradual introduction of the drug and, if necessary, temporary withdrawal of milk products from the diet. Despite theoretical concerns, there is no evidence that colchicine causes infertility or birth defects, and it can be taken safely by nursing mothers. Colchicine has now been licensed by the US Food and Drug administration for the treatment of FMF from the age of 4 years upwards.
Tumour necrosis factor receptor associated periodic syndrome (TRAPS)
Tumour necrosis factor receptor associated periodic syndrome (TRAPS) is very rare and affects about 1 person in a million in Europe. It is an autosomal dominant disease associated with mutations in tumour necrosis factor receptor superfamily 1A gene(TNFRSF1A). As only one abnormal copy of the gene is required to cause disease many patients have family members who also have the disease.
TRAPS was described in 1982 as familial Hibernian fever, but TRAPS has been reported in many ethnic groups. Both sexes are equally affected and symptoms usually start before the age of 4 years. TRAPS attacks are often far less distinct than in FMF. Fever episodes last for weeks and symptoms are near continuous in a third of patients. More than 95% of patients experience fever, and 80% have limb pains that may slowly move inwards towards the chest or abdomen; abdominal pain occurs in 80%, and rash occur in 70% of patients. Other features of attacks include headache, chest pain, enlarged glands and red and swollen eyes. Attacks are accompanied by blood test abnormalities showing inflammation, including high white cells, and a very high C-reactive protein (CRP). Genetic testing is necessary to making a diagnosis.
Acute attacks can be stopped by high dose corticosteroids but this does not stop further attacks from occurring. In more severe disease long term treatment with injected drugs, which block some of the messengers of inflammation, can be very effective in preventing attacks.
Mevalonate kinase deficiency (MKD/HIDS)
Mevalonate kinase deficiency (MKD), also known as Hyperimmunoglobulin D and periodic fever syndrome (HIDS), is an autosomal recessive disease caused by mutations in the mevalonate kinase (MVK) gene. About 60 different mutations have been described and most patients will have a change in both copies of their gene.
MKD is extremely rare and is most often seen in people from North Western Europe. The disease occurs equally in both sexes and usually starts in the first year of life. Attacks are irregular, typically lasting three to seven days, and can be provoked by vaccination, minor trauma, surgery or stress. Symptoms during attacks include fever, enlarged gland in the neck and abdominal pain with vomiting and diarrhoea. Headache, aching limbs, large joint arthritis, rash and mouth ulcers are also common. Attacks are accompanied by blood test abnormalities showing inflammation, including high white cells, and a very high C-reactive protein (CRP).
Treatment is largely aimed at controlling the fever, pain and sickness during attacks but long term treatment with injected drugs, which block the messengers of inflammation, can be very effective in preventing attacks.
Cryopyrin associated periodic syndrome (CAPS)
Most reported patients with cryopyrin associated periodic syndrome (CAPS) have European ancestry but cases have been described from South Asia and elsewhere. The disease usually starts in early infancy, often from birth. Milder disease is typically recurrent episodes of fever, limb aching, red eyes and rash brought on by cold or wet weather. In mid severity disease attacks of fever, aching, non-itchy urticarial rash (looks a bit like ‘nettle rash’) and often headache occur every day, usually from the afternoon onwards. Up to 40% of these patients will develop deafness. The most severe form of CAPS is known as CINCA (chronic infantile neurological, cutaneous and articular syndrome) or NOMID (neonatal onset multisystem inflammatory disease). This is a very severe inflammatory disorder that presents soon after birth. Along with the other features of CAPS there is often destruction of joints and inflammation of the lining of the brain resulting in brain damage, blindness and deafness.
CAPS is caused by mutations in the NLRP3/CIAS1 gene. The disease is dominant and about 75% of patients with milder disease have affected relatives. CINCA, at the most severe end of the clinical spectrum, is usually due to new mutations and there are usually no affected relatives.
Attacks are accompanied by blood test abnormalities showing inflammation, including high white cells, and a very high C-reactive protein (CRP).
There is now very successful treatment for CAPS but this has to be given as injection of drugs which block the messenger of inflammation called IL-1. We run the national treatment centre for CAPS using canakinumab a drug that blocks IL-1 and has to be injected under the skin every 8 weeks. We hope that early treatment may prevent development of complications of CAPS such as deafness and eye damage.
The following diseases are very rare with only a few families known in the world
Deficiency of the IL-1 receptor antagonist (DIRA)
This disease was first described in 2009. It is due to mutations in the IL1RN gene and begins immediately after birth with a rash, joint swelling, and bony swellings in the ribs and the long bones of the arms and legs. It responds very well to treatment with injected drugs.
Pyogenic sterile arthritis, pyoderma gangrenosum and acne (PAPA) syndrome
This exceptionally rare disease is caused by mutations in the PTSTPIP gene. It causes severe acne and recurrent joint swelling typically after minor knocks or damage. Early reports suggest that injected therapies may be effective.
Blau syndrome
This causes rash, joint damage and eye inflammation. Treatment is usually with corticosteroids. It is caused by mutations in NOD2/CARD15.
Periodic fever, aphthous stomatitis, pharyngitis and adenitis (PFAPA)
This was first described in 1987 in a dozen otherwise healthy children. The diagnosis is suggested by the presence of a recurrent fever before the age of 5 years and at least one of the following: mouth ulcers, enlarged glands in the neck or a sore red throat, without an infection. Children are entirely well between attacks and their parents frequently report that they seem less susceptible than other children to minor viral infections. Boys are slightly more affected than girls and it may be commoner among those of European ancestry. The diagnosis is clinical and there is no special test for PFAPA. Attacks are accompanied by blood test abnormalities showing inflammation, including high white cells, and a very high C-reactive protein (CRP). In general most children will outgrow their symptoms within a decade.
Features which suggest a diagnosis of PFAPA are extremely regular and predictable attacks (although there may be some skipping of attacks, particularly in the summer months) and the response to a small dose of corticosteroids. The first line treatment of PFAPA is a single dose of corticosteroid given at the start of the attack. Colchicine has been tried in PFAPA with variable reports of success but our experience has been favourable and it is our first choice of drug. In some children removing their tonsils can stop the attacks completely.
Schnitzler’s syndrome
This adult disease causes a chronic urticarial rash (looks a bit like ‘nettle rash’), fatigue and fever. It usually starts around the age of 50 years or older. Affected patients have an underlying minor bone marrow disease and their plasma cells make too much of an antibody protein, called IgM. This appears to be the cause of Schnitzler’s syndrome although exactly how is not yet clear. Chemotherapy treatment of the bone marrow is not helpful in stopping the rash and fever, although about a fifth of patients eventually develop cancerous bone marrow disease that needs treatment in its own right and may require chemotherapy then.
The treatment of choice of Schnitzler’s syndrome is injected drugs which block a messenger of inflammation called IL-1 and completely prevents all the symptoms
FCAS2
Familial Cold Autoinflammatory Syndrome Type 2 (FCAS2) is a periodic fever syndrome which was first described in 2008 and is a mutation of the NLRP12 gene. There are 37 known patients in the world and two here in the United Kingdom who are members of our group. Although each patient is different symptoms include fever, preceding chills, associated with profuse sweating, often occur at night. Moderate to severe, painful to the touch, skin rash. Moderate to severe myalgia (muscle pain). Moderate to severe arthralgia (joint pain) including stiffness and swelling of the hip, knee and ankle. Moderate to severe headache. Nausea, Drowsiness, extreme thirst during and leading up to flares, Frequent conjunctivitis, blurred vision and eye pain. Moderate glandular pain, hip joint effusion (fluid on the hip), sever penile and scrotum swelling and discolouration. Treatments to help alleviate symptoms are all biologics (Anakinra, Tocilizumab, or Ilaris) which leave patients immunodeficient..
The condition is inherited in an autosomal dominant pattern from an affected parent; one copy of the altered gene in each cell is sufficient to cause the disorder
Long term outcomes
Although CINCA/NOMID and DIRA can be sufficiently severe to cause death within the first few decades, life expectancy among many patients with autoinflammatory disorders is good, and is expected to be excellent in those for whom there is now effective therapy. Most people on treatment will lead completely normal lives. The most serious and life-threatening complication of these diseases generally is AA amyloidosis.
Last Updated on




